The fact that we can now feed our babies breast milk (even without the baby nursing) is amazing.
But what if all of a sudden you find that your breasts suddenly not responding to the pump anymore?
Perhaps it’s been 10 minutes, and you still haven’t had a letdown.
Or maybe you have, but it’s only a few drops.. or more but still waay less than you normally get in one pumping session.
It can be frustrating to see your supply suddenly drop.
Out of nowhere, you’re hit with this sense of dread. How will I be able to feed my baby now?!
I’ve been there too. And to be honest with you, this happens quite often.
Whether you’ve just recently started pumping or have been pumping for several months now, this is something that every pumping mom must have encountered at least once.
So what can you do?

Questions To Ask Yourself
To help you understand what’s causing this issue, ask yourself these questions.
1. How many weeks postpartum are you?
First 6-8 weeks postpartum
If you’re in the early days/weeks, that means you haven’t regulated yet. Your milk supply is primarily dictated by hormones. It can take awhile for your body to adjust to the pump. You’ll have to experiment with different settings, switch between letdown mode and expression mode (most pumps have this feature), change suction strength and speed levels.
After 6-8 weeks postpartum
You’re most likely regulated by this time.[1] That means, your supply going forward will be primarily driven by how often you empty your breasts (whether through pumping or nursing). At this point, you will have to simulate prolactin high through round-the-clock pumping. If you miss a pumping or nursing session, it can potentially impact your supply.
2. Is your period back?
Personally, I got my period back two months postpartum. And when I did, I struggled even more with my supply. It took me longer to get a letdown.
Sometimes, I’d be pumping for 15 minutes and still nothing. I panicked.
After hours of research, I came across this recommendation by La Leche League International (LLL) to take a 500-1,000mg calcium and magnesium supplement everyday from the middle of your cycle (ovulation) right through the first three days of your period.[2]
I followed that and it somehow helped minimize the drop in my milk supply.
Although I can’t quite figure out HOW calcium supplementation helps menstrual-related supply dips, the LLL advice is in line with international recommendations on daily calcium intake for breastfeeding women.[3,4]
3. Have you measured your nipple size recently?
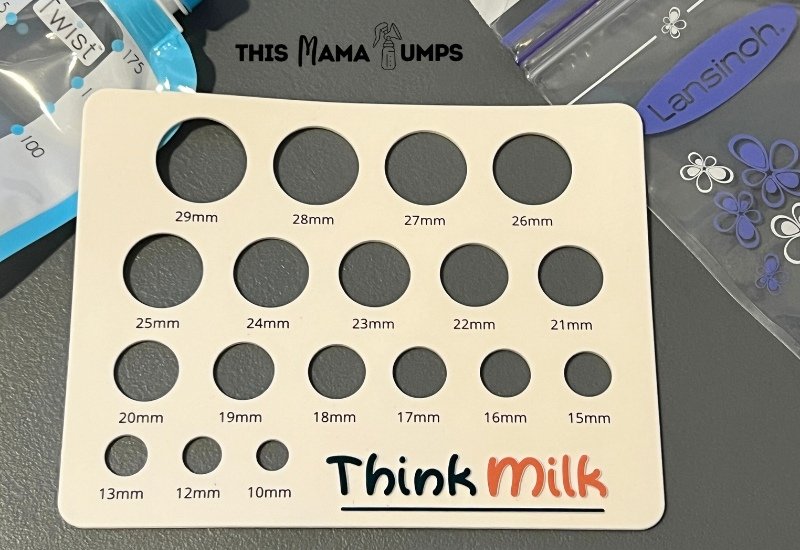
Nipple size during postpartum can change every few months or so.
So what to do?
Have a flange fitting done. But if you prefer to DIY, you can get a silicone nipple ruler to measure your nipple size.
📌 TIP: Use inserts instead of getting a smaller sized flange. They’re way cheaper!
4. Are you using a new pump?
If you just switched to another brand of pump, it takes time before your body gets used to it.
Give it at least 5 days with the new pump before deciding to call it quits. Try different settings, speed, vaccuum strength.
Some pumps like the Spectra S1 and Pumpables Super Genie have a lot of customization options so you get more flexibility. On the flip side, having a lot of options to choose from can be daunting if you’re just starting out!
The good news is, you can find optimal setting recommendations for almost every pump out there. Use Google and Facebook Groups for this.
5. Have you checked your pump parts for wear and tear?
With all the washing and sterilizing, pump parts such as valves and membranes break down with repeated use.
You need to replace them every 3-4 months, depending on how often you use them.
6. Have you checked your pump’s suction?
Pumps can lose suction over time, especially if you’re exclusively pumping (or pumping 8 times or more per day).
Depending on the pump you have, you can send it over for cleaning at the service center. Most breast pump brands recommend yearly cleaning of the pump motor.
7. Are you under stress lately?
I know, i know.
You may be asking, isn’t having a baby a source of stress already?
But what I’m talking about here is a new type or source of stress. Maybe you’re returning to work soon? Perhaps there’s conflict in your family. Or maybe you’re struggling to find childcare options.
Stress can be unavoidable. What matters is how you handle it.
And when you’re a new mom and you’re lacking support, it can be tough. Ask for help. Ask your partner (or a friend or family member) to take over the baby for a few hours.
Go out for a walk. Take deep breaths. Get a massage. Stress management is personal. DO what works for you.
Just to be clear, there’s no evidence that stress directly lowers milk supply. What stress does is put your body in “fight or flight mode” which inhibits oxytocin release (which is necessary for “letdown”).
Simply put, your breasts will have a hard time letting go (“let down”) of the milk it made. And when the milk just sits in the ducts, your body will produce less milk over time.
Rachel O’brien has a good analogy of the “caveperson and the sabre tooth tiger” which explained well the impact of stress on breastfeeding.[5]
8. Are you eating enough calories?
Making milk takes a toll on our bodies. It takes a lot of calories to make milk! No wonder we’re constantly feeling hungry while breastfeeding. If you don’t eat enough calories and nutrients, your supply will dip.
I totally get it if you want to start dieting.
However, when you’re still breastfeeding, you need those carbs.
Not the pasta, cake and chocolates, mind you. But those healthy, whole-food carbs found in fruits and vegetables.
If you still want to go low-carb, do it slow.[6]
Don’t just suddenly drop your caloric intake. It’s also best to work with a registered dietician or nutritionist who can personally guide you.
9. Are you drinking enough water or fluids?
Hydration is very important in breastfeeding.[7]
Have you recently been drinking tea or coffee (which can dehydrate you)? Drinking less water (or fluids, in general)?
That could explain why your supply is dipping, and as a result, your body is not responding to the pump like you used to.
Despite lack of evidence, hydration drinks like Body Armor continue to be a staple drink of many pumping moms. It’s not that they actually increase milk supply. It’s that they give your body the extra fluids it needs to produce milk.
Of course, there’s water. Personally, I’m more of a water person myself. I bring a tumbler of water with me wherever I go.
But I get that there are people who prefer flavored drinks and so these hydration drinks are perfect for them.
When To Seek Professional Help
I hope you found the questions above somehow helpful. But if you’ve gone through that list and still can’t figure out what’s causing your issues, it might be best to see a lactation consultant for a more personalized advice.
Peer Support
It can be tough to get the support you need, especially if you personally don’t know anyone else who pumps.
Thankfully, we have the internet and social media. I created a list of online pumping and breastfeeding support groups – check it out here.
This list is a work-in-progress so please check back from time to time.
I Wanna Hear From You!
If you’ve tried any of the tips I mentioned above, I’d love to hear from you. Perhaps you also have another tip which worked for you. Feel free to leave a comment below.
Remember, breastfeeding is not “all or nothing”.
You’re doing a GREAT JOB whether you’re pumping 1.5 ounces or 5 ounces.
References:
- Jessica Anderson, IBCLC, CLC. The Infamous 12-Week Supply Regulation. https://www.genuinelactation.com/blog-for-breastfeeding-families/the-infamous-12-week-supply-regulation
- La Leche League International 2021. Menstruation. https://llli.org/breastfeeding-info/menstruation/
- Carretero-Krug, A., Montero-Bravo, A., Morais-Moreno, C., Puga, A. M., Samaniego-Vaesken, M. L., Partearroyo, T., & Varela-Moreiras, G. (2024). Nutritional Status of Breastfeeding Mothers and Impact of Diet and Dietary Supplementation: A Narrative Review. Nutrients, 16(2), 301. https://doi.org/10.3390/nu16020301 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10818638/
- Thomas, M., & Weisman, S. M. (2006). Calcium supplementation during pregnancy and lactation: effects on the mother and the fetus. American journal of obstetrics and gynecology, 194(4), 937–945. https://doi.org/10.1016/j.ajog.2005.05.032 https://pubmed.ncbi.nlm.nih.gov/16580279/
- Rachel O’Brien, IBCLC 2017. Stress and Breastfeeding: How to Protect Your Milk Supply. https://www.rachelobrienibclc.com/blog/stress-and-breastfeeding-protect-milk-supply/
- Kelly Bonyata, IBCLC 2023. Low Carb Diets and Breastfeeding. https://kellymom.com/nutrition/mothers-diet/mom-lowcarb/
- Barbara Gordon, RDN, LD 2022. Academy of Nutrition and Dietetics. Nursing Your Baby — What You Eat and Drink Matters. https://www.eatright.org/health/pregnancy/breastfeeding-and-formula/nursing-your-baby-what-you-eat-and-drink-matters

